By Ken Grauer, MD
Professor Emeritus in Family Medicine, College of Medicine, University of Florida
The ECG in the figure below was obtained from a previously healthy young woman with “palpitations.” How would one interpret this two-lead rhythm strip? Is there a conduction disorder?
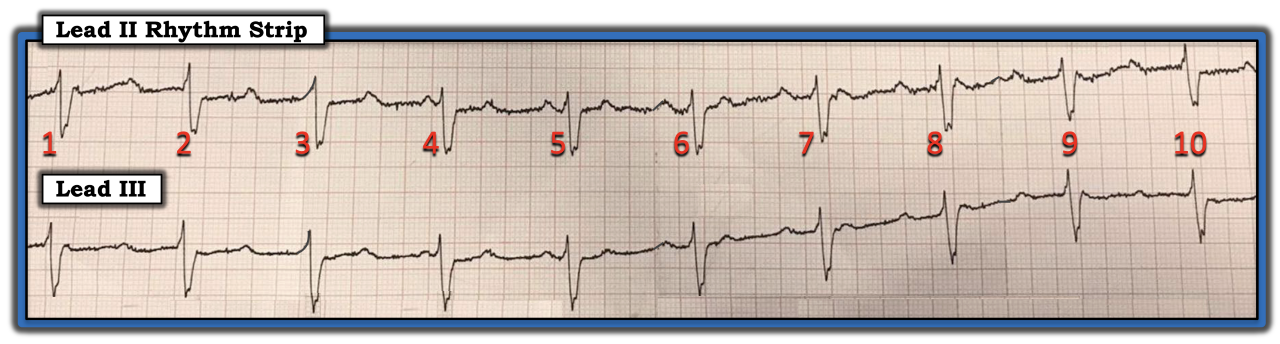
There are several reasons why it is challenging to interpret this strip. There is a significant amount of baseline artifact in both leads. Atrial activity is partially (or completely) hidden in many places. The QRS complex is wide, but there is no 12-lead ECG to help assess the origin of ventricular complexes. There is no obvious relationship between P waves and neighboring QRS complexes for the 10 beats that are visible.
As always, once ensuring the patient is hemodynamically stable, I address five ECG parameters for interpreting the rhythm. Use of the memory aid “watch your Ps, Qs, and the three Rs” facilitates remembering these parameters. P waves clearly are present in this tracing. The challenge entails finding all the P waves that are hidden within parts of the ST-T wave or QRS complex. In my experience, using calipers is the most time-efficient way to find hidden P waves and to determine if the atrial rhythm is regular. Find a place on the rhythm strip where two P waves in a row are visible and set the calipers to this P-P interval. Then, try to walk out P waves from that point on the strip. For example, two P waves appear to be seen in lead III within the R-R interval between beats 6-7, 7-8, and 8-9.
There is deflection in lead III that occurs right after the QRS complex for beats 7, 8, and 9; there is no such deflection at a similar point after the QRS complex of beats 2-6. This “extra” deflection is visible again right after the QRS complex of beat 1. Setting the calipers to the P-P interval suggested by any of the noted two consecutive P waves allows one to walk out regular atrial activity at ~130 beats per minute throughout this strip. The QRS complex is wide and regular at ~60 beats per minute. Unfortunately, without seeing a complete 12-lead ECG, it is impossible to tell if the reason for QRS widening is a supraventricular conduction defect vs. a ventricular escape rhythm. Looking in front of each QRS complex suggests the PR interval continually changes.
The finding of a regular atrial rhythm and a regular ventricular rhythm (but a continually changing PR interval) suggests none of the P waves on this 10-beat rhythm strip are conducting. The rapid atrial rate of ~130 beats per minute suggests an underlying atrial tachycardia. The regular ventricular rhythm without evidence of conduction suggests ventricular escape, either arising from the AV node or from a slightly accelerated ventricular escape rhythm.
Without a longer period of ECG monitoring, it is impossible to determine if the conduction defect represents high-grade or complete AV block. That said, there is at the least a high-grade AV block in a previously healthy young adult woman who manifests a wide QRS escape rhythm. Further evaluation is indicated to determine the underlying reason for this severe conduction defect.
For further discussion on and information about this case, including step-by-step laddergram illustrations, please click here.
The ECG in the figure was obtained from a previously healthy young woman with “palpitations.” How would one interpret this two-lead rhythm strip? Is there a conduction disorder?
You have reached your article limit for the month. Subscribe now to access this article plus other member-only content.
- Award-winning Medical Content
- Latest Advances & Development in Medicine
- Unbiased Content